👉👉 🇺🇸 All Posts 🇬🇧 / 🇯🇵 記事一覧 🇯🇵 👈👈
♦️ Introduction
 まっすー
まっすーHave you ever seen a real case of LAST?



Just once—back when I was a resident. Rare, but when it happens, it’s serious. That’s why we practice.



The lipid emulsion—that’s the white bag in the crash cart, right?



Exactly. You should be able to grab it in seconds. For an average adult, you’ll probably need one full pack.
Local Anesthetic Systemic Toxicity (LAST) is uncommon but potentially life-threatening.
With prompt recognition and early lipid emulsion therapy (Lipid Emulsion Therapy: LET), the prognosis has improved dramatically.
The American Society of Regional Anesthesia and Pain Medicine (ASRA) provides a stepwise checklist that has become the international standard for LAST management.
This article summarizes the clinical workflow and exam-relevant key points.
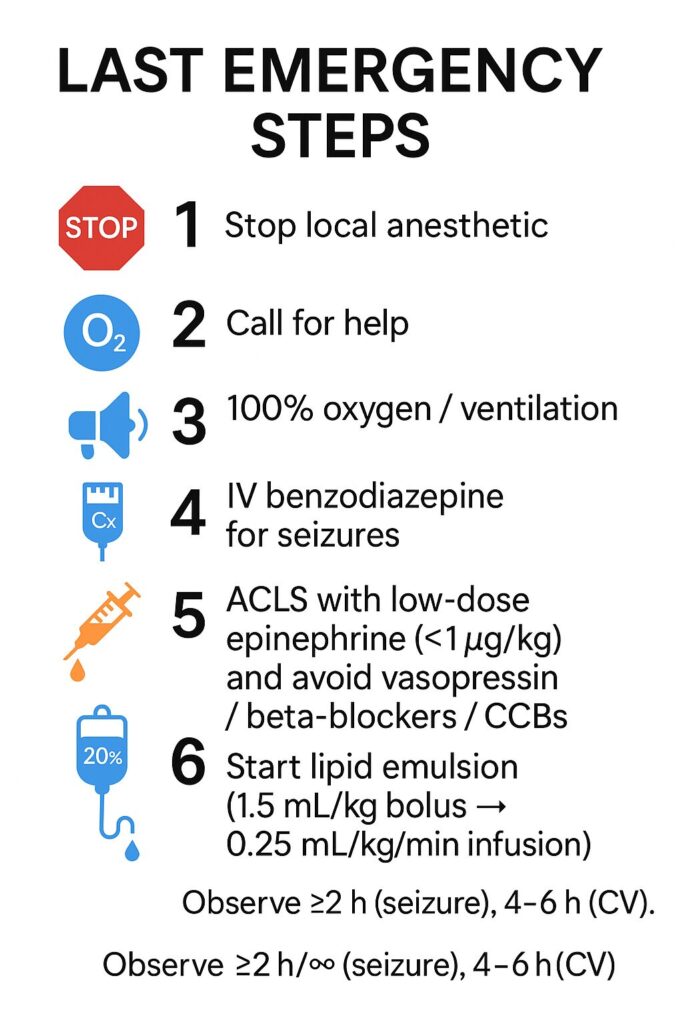
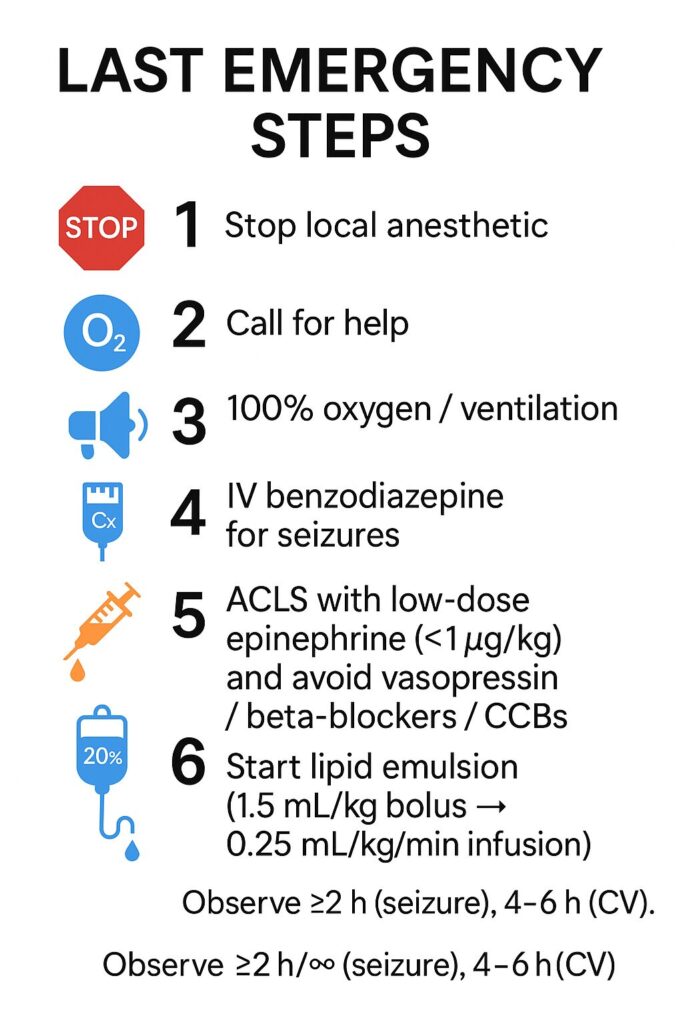
♦️ Immediate Management ( ASRA-based )
🔷 Stop the infusion and call for help 🔈
- Immediately stop administration of the local anesthetic and activate the emergency response.
Continuing the injection while “just watching” is dangerous.
If you are performing a block, stop the syringe or pump first.
If using a catheter infusion, clamp the line immediately—this single action can save a life.
🔷 Airway and breathing 🫁
- Provide 100 % oxygen and ensure adequate ventilation.
- Prevent hypoxia and acidosis, which worsen cardiotoxicity.リスト
🩺 Clinical note:
Acidosis and hypercapnia increase the unbound fraction of local anesthetic in plasma, amplifying toxicity.
Mild hyperventilation to maintain normal pH is recommended.
📘 Exam tip:
“If asked for the first step in LAST management” → oxygenation and ventilation is the correct answer.
🔷 Seizure control ⚡️
Treat seizures promptly with intravenous benzodiazepines (midazolam or diazepam).
Avoid large doses of propofol or barbiturates, which can cause cardiac depression.
🩺 Clinical note:
Propofol has anticonvulsant properties but also reduces myocardial contractility—creating a “double hit.”
Use benzodiazepines first and maintain ventilation.
📘 Exam tip:
“Which agents should be avoided?” → High-dose propofol and barbiturates.
🔷 Cardiovascular collapse or arrhythmia
Follow ACLS principles, but with key modifications:
- Use low-dose epinephrine (< 1 µg/kg)
- Avoid vasopressin, β-blockers, and calcium channel blockers
- For antiarrhythmics: lidocaine is contraindicated; amiodarone is acceptable
🩺 Clinical note:
High-dose epinephrine increases myocardial oxygen demand and may worsen reperfusion injury.
These drugs differ from standard ACLS because their hemodynamic effects compound the toxicity.
📘 Exam tip:
“Which ACLS modifications are correct for LAST?” → Low-dose epi, no vasopressin, no lidocaine.
🔷 Refractory or Delayed Cases
If there is no response to LET + ACLS, consider ECMO or cardiopulmonary bypass early.
Bupivacaine toxicity, in particular, carries a risk of recurrent collapse—patients should be observed in the ICU for extended monitoring.
♦️ Lipid Emulsion Therapy (LET)
🔹 When to start
Initiate as soon as severe CNS symptoms (e.g., seizures, unconsciousness) or any cardiovascular instability appear.
As NYSORA emphasizes: “Do not wait for cardiac arrest.”
🔹 Standard ASRA regimen
- 20 % lipid emulsion, 1.5 mL/kg IV bolus over 2–3 min
- Continue infusion at 0.25 mL/kg/min
- If instability persists → repeat bolus or double infusion rate (0.5 mL/kg/min)
- Maximum total dose: ~10–12 mL/kg (follow institutional protocol)
🩺 Clinical note:
The lipid emulsion not only creates a “lipid sink” to sequester lipophilic drugs but also improves myocardial metabolism and contractility.
Early administration correlates strongly with survival.
📘 Exam tip:
“Initial bolus dose of lipid emulsion?” → 1.5 mL/kg (20 %).
♦️ Prognosis
- Early LET yields > 90 % survival
- Most patients recover fully without neurologic sequelae
- Delayed or infusion-related cases carry worse outcomes
- Registry data show mortality < 10 % since LET became routine
🩺 Clinical note:
Even after hemodynamic recovery, neurologic symptoms may lag for several hours.
Maintain observation for at least 2 h after seizures and 4–6 h after cardiovascular instability.
♦️ Team Training and Preparedness
- Display the ASRA LAST checklist in every block room, OR, and ED.
- Keep a “LAST kit” stocked (20 % lipid emulsion, dosing chart, syringes, tubing).
- Conduct simulation training once or twice a year.
The educational focus:
- Initiate lipid early, and
- Remember the ACLS differences.
📝 Summary : Take-Home Points
- Stop, call, oxygen — act simultaneously.
- Seizure → benzodiazepine; avoid high-dose propofol.
- Low-dose epinephrine only; no vasopressin, β-blockers, or CCBs.
- Lipid emulsion: 1.5 mL/kg bolus → 0.25 mL/kg/min infusion (> 15 min).
- > 90 % recover with early LET.
- Checklist + education + kit = the best prevention.リストリスト
📚 References & Further reading
- ASRA. Checklist for Treatment of Local Anesthetic Systemic Toxicity (2020).
- StatPearls. Local Anesthetic Toxicity (2022).
- NYSORA. Local Anesthetic Systemic Toxicity (2024).
- El-Boghdadly K et al. Local anesthetic systemic toxicity: current perspectives (PMC 2018).
- Weinberg G. APSF 2024 Update: LAST Revisited (Open Access).
- Liu Y et al. Frontiers in Medicine 2021 – Mechanisms of lipid emulsion.
All protocols should follow institutional guidelines. Doses and thresholds shown are derived from ASRA 2020 and major open-access reviews.
コメントを投稿するにはログインしてください。