👉👉 🇺🇸 All Posts 🇬🇧 / 🇯🇵 記事一覧 🇯🇵 👈👈
Type & Screen
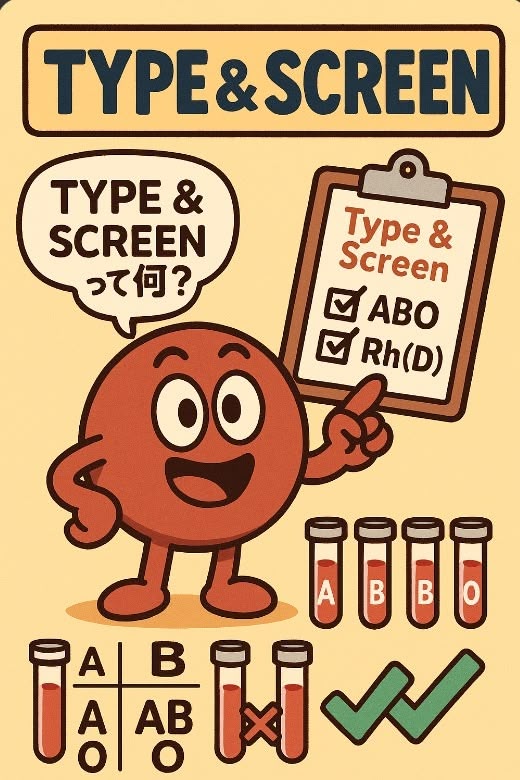
🔷 What is “Type & Screen”?
You may have seen “Type & Screen” in pre-admission blood work.
In short, it is a method of preparing for transfusion in an efficient way.
When a surgery is expected to involve possible but not certain blood transfusion—for example, “maybe just a little bleeding, maybe none at all”—the patient’s ABO blood type and irregular antibodies are checked in advance. Blood is then “reserved” for that patient but not physically crossmatched. If transfusion becomes necessary, it can be quickly used. If not, the blood can be reassigned to another patient.
🔷 Are there criteria?
Generally, Type & Screen is used when:
- The probability of transfusion is less than ~30%, or
- Expected transfusion volume is 2 units or less.
(Note: Exact thresholds vary by institution and country. For example, the AABB [American Association of Blood Banks] provides guidance, but hospitals may set their own criteria.)
If the antibody screen is negative, crossmatching can be omitted and only ABO compatibility confirmed.
Crossmatch (Compatibility Testing)
🔷 What is a “crossmatch”?
The crossmatch (pre-transfusion compatibility testing) is performed to prevent fatal ABO-incompatible transfusions. It is usually performed in the blood bank or laboratory.
🔷 Major vs. Minor crossmatch
- Major crossmatch: recipient serum vs. donor red cells
- Minor crossmatch: recipient red cells vs. donor serum
However, modern red cell components are almost plasma-free. Because donor plasma is largely removed, the minor crossmatch has little clinical significance and is now omitted in most institutions.
Thus, the major crossmatch remains the key test.
If the major crossmatch is positive, transfusion should not proceed. In emergencies, uncrossmatched group O (Rh-compatible) blood is used instead.
Irregular Antibodies
🔷 What are “irregular” antibodies?
- Regular antibodies: naturally occurring anti-A and anti-B (present in almost everyone, predictable).
- Irregular antibodies: all others against red cell antigens; not naturally present, but may develop after transfusion or pregnancy, and thus are unpredictable.
There are over 200 types of irregular antibodies. The most clinically important are:
- Rh system antibodies (C, c, D, E, e) — anti-D is the strongest, anti-E is also important
- Kell antibodies — also highly significant in transfusion and pregnancy
RhD-negative Patients
🔷 Hemolytic Disease of the Newborn (HDN)
If an RhD-negative mother carries an RhD-positive fetus, fetal blood may enter maternal circulation at delivery. Maternal anti-D antibodies then develop. The first child is rarely affected, but subsequent pregnancies may result in hemolytic disease of the newborn.
Prevention: anti-D immunoglobulin within 72 hours after delivery (standard worldwide).
🔷 Emergency Massive Transfusion
If RhD-negative blood is unavailable in emergencies, RhD-positive red cells may be given to save life. Once RhD-negative blood is available, transfusion should be switched immediately.
- For women of childbearing age, this is especially critical, as alloimmunization may cause hemolytic disease in future pregnancies.
- After emergency RhD-positive transfusion, antibody screening should be performed within 48 hours. If anti-D is negative, anti-D immunoglobulin may be administered (though efficacy may be limited). If anti-D has already formed, delayed hemolytic transfusion reactions may occur and close monitoring is needed.
🔷 Common Question: Antigens vs. Antibodies
Some people ask: “If someone has the D antigen, do they also have anti-D antibodies? Why doesn’t a reaction occur?”
The answer: antibodies form only against what is recognized as “non-self.” Your own D antigen is “self,” so you do not make anti-D. This is called immune tolerance. Therefore, RhD-positive people do not have anti-D antibodies and can safely receive RhD-positive blood.
📝 Summary
- Type & Screen: Used when transfusion is unlikely but possible. Test ABO type and screen for irregular antibodies; reserve blood efficiently.
- Crossmatch: Prevents fatal incompatibility. Today, minor crossmatch is obsolete; the major crossmatch remains essential.
- Irregular antibodies: May form after transfusion/pregnancy. >200 types exist; most important are Rh system (especially D, E) and Kell.
- RhD-negative patients: Risk in pregnancy (hemolytic disease of the newborn) and emergency transfusions. Prevention by anti-D immunoglobulin is standard.
- Immunology: Antibodies form against “non-self.” People with D antigen do not have anti-D antibodies.
🔗 Related articles
- 🩸 Platelet Transfusion — Why Do We “Shake” Platelet Concentrates?
- 🩸Autologous Blood Transfusion Explained: What You Need to Know Before Surgery
- 🩸Has the FFP thawed yet?🫠
- 🩸Red Blood Cell Transfusion (RCC) ~Will the bleeding stop? Surgeon says yes… Anesthesiologist says 🤔
- 🩸What Are Blood Types A, B, O, and AB?
- 🩸What do the labels “lr” and “LR” on blood products mean?
コメントを投稿するにはログインしてください。