👉👉 🇺🇸 All Posts 🇬🇧 / 🇯🇵 記事一覧 🇯🇵 👈👈
♦️ What is Radiation?
Simply put, radiation is invisible energy that travels through space.
Think of it like this: if a fist 👊 (a visible form of energy) hits your face, you’ll see swelling or bleeding right away😅. Radiation, on the other hand, is invisible energy — when absorbed by our body it can also cause damage. But unlike a punch, sometimes the effects show up much later.
(Here we’re talking about ionizing radiation — like X-rays or gamma rays — the kind used in medicine or nuclear science. Non-ionizing radiation such as radio waves or infrared light is not the focus here.)
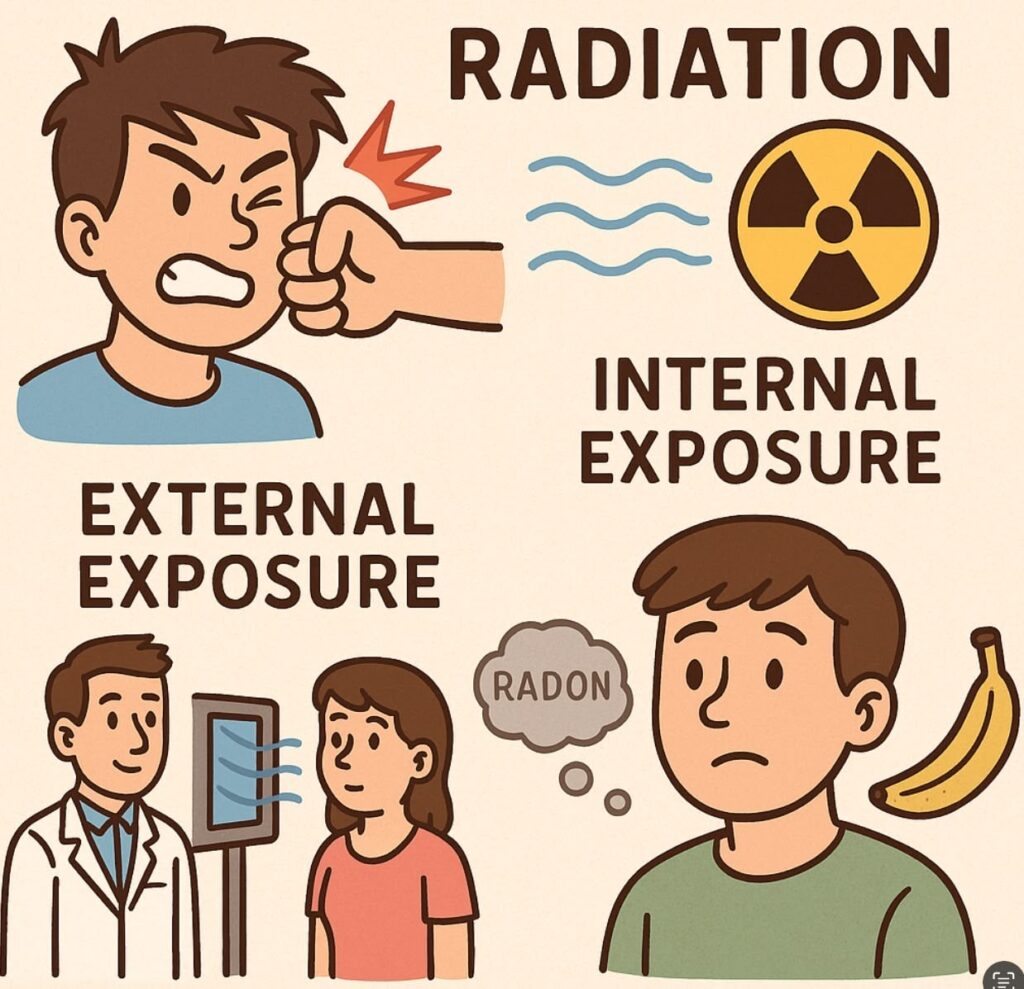
♦️ Types of Exposure ①: External vs. Internal
- External exposure: This is when radiation comes from outside the body. Typical examples are chest X-rays, CT scans, or radiation from catheter-based procedures.
- Internal exposure: This occurs when radioactive materials enter the body through food, drink, or inhaled gases (like radon). Radioactive iodine (I-131), which became an issue after nuclear accidents, is another example.
♦️ Types of Exposure ②: Public, Medical, and Occupational
🔷 Public Exposure
Radiation is all around us, even in nature.
- Cosmic rays from space
- Terrestrial radiation from soil and rocks
- Food (for example, bananas contain potassium-40 🍌)
This unavoidable background is called natural radiation exposure.
In addition, exposure can come from man-made sources such as nuclear power plants, laboratories, or industrial facilities. All of this combined is called public exposure.
👉 Unless there is a major nuclear accident, natural and public exposure levels are too low to cause health problems.
🔷 Medical Exposure
Medical exposure refers to radiation received by patients during diagnostic imaging or treatment.
This includes plain X-rays, CT scans, or radiation therapy using gamma rays.
Here’s the key difference: unlike occupational exposure, there is no dose limit for patients.
Why? Because:
- The benefits of the examination or treatment outweigh the risks of radiation exposure.
- Each patient’s condition is different, making a universal dose limit impractical.
That said, unnecessary exposure should always be minimized. For example, during catheter-based interventions, protective devices are used to reduce exposure to non-target areas such as the gonads.
🔷 Occupational Exposure
This is the type of exposure faced by healthcare professionals and workers who handle radioactive materials.
Since some exposure is unavoidable, dose limits are set for workers (annually, and for women of reproductive age, also within 3-month periods).
In medical practice, patients receive the primary beam, but some radiation:
- reaches detectors,
- is absorbed by tissue, and
- scatters in different directions (scatter radiation).
👉 Healthcare workers are mostly exposed to this scatter radiation.
To monitor exposure, workers wear personal dosimeters such as:
- Glass badge dosimeters (checked monthly),
- Ring dosimeters (especially for interventionalists),
- Electronic dosimeters (which allow real-time monitoring).
As long as protective equipment is used properly and monitoring is performed, exceeding the dose limits is very rare.
🔷 Summary
- Radiation is a part of everyday life — it’s impossible to avoid completely.
- In medicine, patients receive radiation when the benefits outweigh the risks, and healthcare workers protect themselves with shielding and careful monitoring.
- The key is to understand radiation correctly: don’t fear it excessively, but don’t underestimate it either. With proper precautions, both patients and healthcare professionals can stay safe.
コメントを投稿するにはログインしてください。