👉👉 🇺🇸 All Posts 🇬🇧 / 🇯🇵 記事一覧 🇯🇵 👈👈
♦️ Introduction
 まっすー
まっすーI once had a patient who said their tongue felt numb right after a brachial plexus block. Nothing else happened afterward, but… is that okay?”



Whoa — that could’ve been an early sign of local anesthetic systemic toxicity (LAST). How long after the injection did it happen?



Within a few minutes.



Depending on the dose, LAST can appear within seconds. You need to stop the injection immediately and check the patient’s consciousness, breathing, and blood pressure right away.


♦️ Overview
Local Anesthetic Systemic Toxicity (LAST) is rare in practice, but when it occurs, it can be life-threatening.
In most cases, symptoms appear within seconds to a few minutes after injection.
They typically begin with central nervous system (CNS) symptoms such as anxiety, tinnitus, perioral numbness, metallic taste, or seizures, and may progress to cardiovascular (CV) symptoms such as bradycardia, hypotension, arrhythmias, and cardiac arrest.
Although reports vary, the estimated incidence during peripheral nerve blocks is approximately 0.03 % (StatPearls 2022; Cleveland Clinic 2025).
Even though the event is rare, progression can be extremely rapid—recognition, stopping the injection, and immediate action often make the difference between recovery and catastrophe.
This article reviews the clinical features, risk factors, and initial management of LAST, written in a practical tone for clinicians and exam preparation alike. 😊
♦️ Onset and Characteristics
In most cases, LAST appears within seconds to minutes after injection. Half of cases occur within 50 seconds, and about 75 % within 5 minutes.
However, delayed toxicity can occur hours later—especially with continuous catheter infusions or highly vascular injection sites (ScienceDirect 2025).
Therefore, even if the patient seems stable right after the block, don’t let your guard down.
For high-risk patients, it’s recommended to observe for at least 30–45 minutes post-procedure.
☝️ There are reports of seizures and cardiac arrest occurring just 50 seconds after a supraclavicular block (StatPearls 2022), whereas other cases developed toxicity several hours later after continuous infusion (ScienceDirect 2025).
In short, LAST can occur either immediately or hours later—so careful monitoring and documentation are essential.
🔷 Central Nervous System (CNS) Symptoms 🧠
The initial stage often manifests as CNS excitation.
If a patient reports tinnitus, dizziness, metallic taste, perioral numbness, or feeling anxious, those are warning signs that the anesthetic plasma level is rising.
If left untreated, this may rapidly progress to generalized seizures, loss of consciousness, respiratory arrest, and coma.
After the excitation phase, a depression phase may follow, with somnolence and respiratory suppression.
Be especially cautious when sedatives are used concurrently, as they can mask these early symptoms.
🔷 Cardiovascular (CV) Symptoms 🫀
Cardiovascular changes typically follow CNS signs, though simultaneous onset can occur if plasma concentration rises abruptly.
Early on, you may see a transient increase in blood pressure and heart rate, followed by bradycardia, hypotension, and ventricular arrhythmias.
Potent cardiotoxic agents such as bupivacaine can cause sudden cardiac arrest without preceding CNS symptoms.
Additionally, agents such as benzocaine, prilocaine, and lidocaine may induce methemoglobinemia, leading to chocolate-colored blood and falsely low pulse-oximeter readings.
🔷 Diagnosis
The diagnosis of LAST is clinical—there is no specific confirmatory test.
The key is to recognize the temporal link between anesthetic injection and characteristic symptoms.
Differential diagnoses include oversedation, hypoxia, hypoglycemia, stroke, and seizure disorders.
When perioral numbness, tinnitus, or seizures occur during or right after injection, it is safest to presume LAST until proven otherwise and begin treatment immediately.
♦️ Risk Factors ✅
Factors that increase the risk of LAST include:
- Age < 6 years or > 60 years
- Low muscle mass
- Cardiac or hepatic dysfunction
- Metabolic disease such as diabetes
These conditions alter anesthetic distribution and metabolism, increasing toxicity risk.
Highly vascular injection sites (intercostal, cervical) and large or high-concentration doses also elevate the risk.
Continuous catheter infusions can cause delayed toxicity hours—or even a day—after injection.
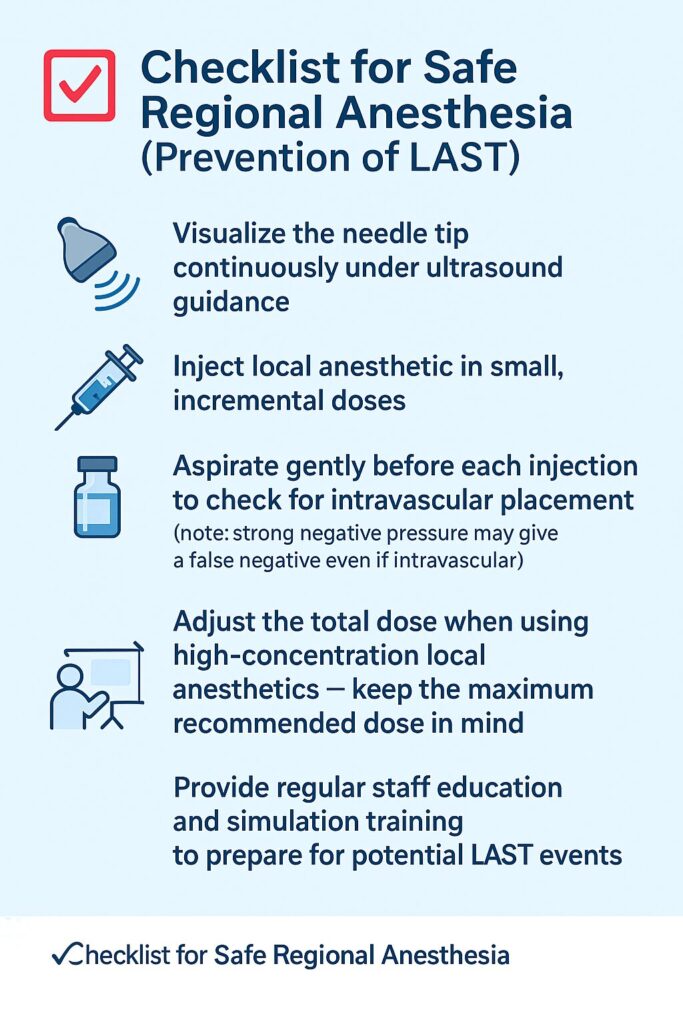
♦️ Prevention ✋
The most effective management is prevention.
Use ultrasound guidance to confirm the needle tip location, and inject incrementally in small aliquots, aspirating before each dose.
Be gentle when aspirating—strong suction may yield a false negative even if intravascular.
When using high-concentration local anesthetics, adjust the total dose according to patient size and risk profile.
Each facility should maintain a visible “LAST Kit” containing lipid emulsion and emergency drugs, along with a posted algorithm so every team member knows exactly what to do.
Regular education and simulation drills make a big difference when seconds count.
♦️ Immediate Management
If symptoms appear, act immediately—do not hesitate.
The following outline is based on the ASRA Checklist (2020) and current international recommendations.
(A detailed discussion of lipid therapy and evidence will appear in a follow-up article.)
- Stop injection immediately and call for help.
- Administer oxygen and secure the airway with bag-mask ventilation or intubation if necessary.
- Control seizures with IV benzodiazepines (e.g., midazolam). Avoid large doses of barbiturates or propofol that can worsen cardiac depression.
- Support circulation: manage bradycardia, hypotension, and arrhythmias following standard ACLS protocols.
- Prepare lipid emulsion therapy: in severe or refractory cases (persistent seizures or cardiovascular collapse), start 20 % intralipid according to your institutional or ASRA protocol.
- Document all details—dose, timing, symptoms, and interventions—and contact toxicology or the ICU team early.
♦️ Summary / Take-Home Points
- Local Anesthetic Systemic Toxicity (LAST) is rare but can progress within seconds to minutes.
- Most cases begin with CNS symptoms (perioral numbness, tinnitus, metallic taste, seizures), but cardiotoxic agents may cause cardiac collapse first.
- Immediate management = Airway + Oxygen + Seizure control + Circulatory support.
- Lipid emulsion therapy can be lifesaving—follow your institutional protocol.
- Prevention through ultrasound guidance, incremental injection, and extended observation remains the most powerful strategy.
📚 References & Further reading
- Mahajan C, et al. Local Anesthetic Toxicity. StatPearls, 2022. NCBI Bookshelf
- Cleveland Clinic. Local Anesthetic Systemic Toxicity (LAST): Symptoms & Treatment. 2025.
- NYSORA. Local Anesthetic Systemic Toxicity. 2024.
- ASRA. Checklist for Treatment of LAST. 2020.
- APSF. Revisiting LAST – A Paradigm Shift. 2021.
- Shalaby M, et al. Delayed Local Anesthetic Systemic Toxicity. ScienceDirect, 2025.
- Practical guide for the management of systemic toxicity caused by local anesthetics. Jounal of Anesthesia 2019 33:1-8
🔗 Related articles
- to be added
コメントを投稿するにはログインしてください。