👉👉 🇺🇸 All Posts 🇬🇧 / 🇯🇵 記事一覧 🇯🇵 👈👈
♦️ Introduction
In the operating room, intubation is usually performed by anesthesiologists. The higher-risk situations occur on the wards during sudden deterioration or in the hectic environment of the emergency department.
This was especially true in the past. Nowadays, the widespread use of video laryngoscopes has significantly reduced the risks, though caution is still required.

♦️ Daily Endotracheal Intubation
Endotracheal intubation is performed countless times every day. On the wards, it is often in the context of a code or sudden deterioration, where less experienced staff may be present or staffing is limited at night. In such situations, things can get quite chaotic.
In contrast, intubation in the operating room is planned, performed in a controlled environment, and rarely chaotic—even when residents perform the procedure.
🔷 The Frightening Complication: Esophageal Intubation
At the back of the throat there are two tubes—one leading to the trachea and one to the esophagus. The trachea lies anteriorly, while the esophagus is behind it. The endotracheal tube must go into the trachea; otherwise, the patient cannot breathe.
Esophageal intubation occurs when the endotracheal tube is mistakenly placed into the esophagus. This prevents oxygen from reaching the lungs, and if unrecognized, can rapidly lead to death.
Unfortunately, there are reports of patients suffering severe harm or even dying when an esophageal intubation went unnoticed—such as in single-specialty hospitals where surgery was performed without anesthesiologist involvement. This must absolutely be avoided.
🔷 Esophageal Intubation Happens – What Matters Is Rapid Recognition
Almost every physician who has performed intubation has experienced an esophageal intubation. Technical difficulty and patient factors can make intubation challenging, even for skilled operators.
So why is this complication rarely catastrophic? Because anesthesiologists recognize it quickly. Mistakes happen in every profession, but what matters is identifying them promptly and correcting course.
♦️ Methods to Confirm Endotracheal Tube Placement
Textbooks and manuals describe several methods for confirming tracheal intubation, often taught by anesthesiologists to residents and nurses. Common ones include:
🔹 Observing chest rise
Simple and quick, but not always reliable—especially in obese patients.
🔹 Auscultation
Listening at multiple points, including the epigastrium. Esophageal intubation may produce gurgling sounds. However, breath sounds can be faint, especially in obese patients or noisy environments.
🔹 Tube fogging
Exhaled humidified air fogs the inside of the tube. Easy to see in the OR, but difficult in dim lighting on the wards.
🔹 Esophageal detector device (EDD)
A bulb or syringe is attached to the tube; if in the trachea, air refills the bulb, whereas in the esophagus it remains collapsed. Simple in concept, but prone to both false positives and false negatives, and not widely relied upon.
🌟 Capnography – the gold standard
Capnography measures exhaled CO₂. A clear waveform strongly confirms correct placement. This is universally available in operating rooms but less so in wards, ICUs, cath labs, and ERs.
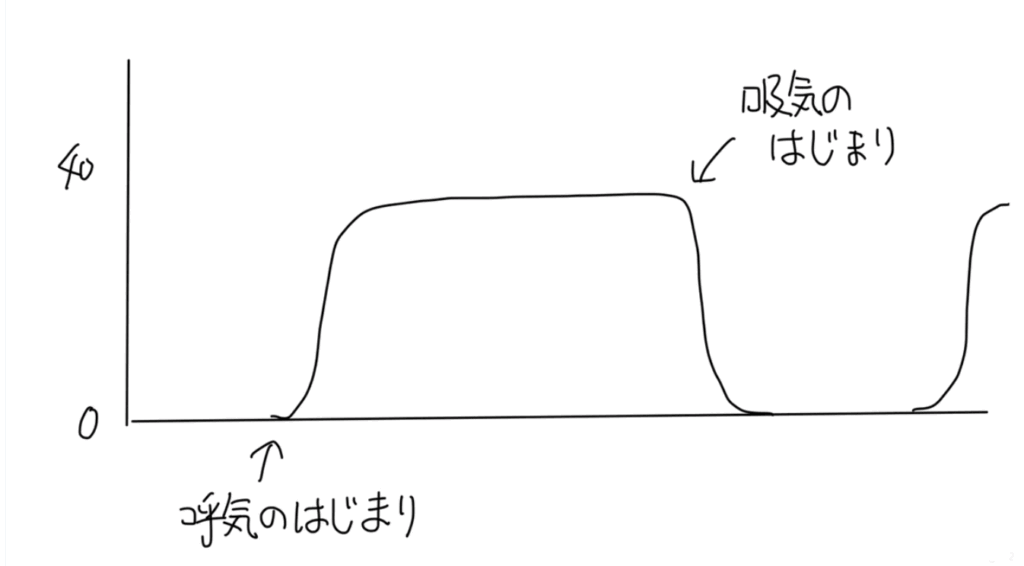
Rarely, false waveforms may appear initially if:
- Mask ventilation insufflated gas into the stomach.
- During chest compressions in cardiac arrest.
- The patient recently consumed carbonated beverages.
⤴️ These waveforms quickly disappear, so attentive monitoring avoids misinterpretation.
🌟 The Game-Changer: Video Laryngoscopes

Capnography remains the most reliable monitor, but since it is not always available outside the OR, video laryngoscopes have become the practical solution.
First introduced around 15 years ago (e.g., the Airway Scope), they are now widely available, with common devices such as the McGRATH. Prices have dropped significantly, and even freelance anesthesiologists often purchase their own.
Video laryngoscopes make intubation much easier, allow clear visualization of the tube entering the trachea, and enable confirmation by multiple observers. They have become widely available in ORs, ERs, and wards. One must, however, ensure batteries are functional.
Another advantage: even if batteries fail, most video laryngoscopes can still function as conventional laryngoscopes.
While anesthesiologists should still maintain skills with direct laryngoscopy, for risk reduction, video laryngoscopy is often the safer choice. Personally, I have used video laryngoscopes almost exclusively over the past decade, and esophageal intubations are exceedingly rare among trainees using them.
🔷 POCUS-based Confirmation of Endotracheal Intubation 🆕✨
In recent years, point-of-care ultrasound (POCUS) has garnered attention in emergency and ICU settings as a supplemental method to confirm endotracheal intubation.
Method Overview
- Place an ultrasound probe over the anterior neck (just above the suprasternal notch) to visualize the tube passing into the trachea (“snowstorm sign” for dynamic movement, or “double tract sign” in esophageal intubation) CEEM Journal+2institutionalrepository.aah.org+2
- Assess lung ultrasound bilaterally to check for lung sliding, which suggests that ventilation is reaching both lungs (indirect confirmation) CEEM Journal+2PMC+2
- Some operators inflate the ETT cuff with saline (instead of air) to improve sonographic visibility or twist the tube slightly to generate motion artifact to aid detection PMC+2institutionalrepository.aah.org+2
Accuracy, Advantages, and Limitations
- In adults, POCUS has been reported to have very high sensitivity and specificity (e.g., ~99 % sensitivity and ~97 % specificity in select studies)
- Compared to auscultation, POCUS can be less affected by ambient noise and operator hearing, making it more reliable in chaotic environments
- Limitations and caveats include:
• Operator skill dependence — requires training and experience
• Air causes acoustic shadowing or artifacts, making visualization difficult in some cases
• It is best used as an adjunct to standard methods (capnography, visualization) rather than a standalone confirmation in all settings
Summary (Take-Home Points)
- Esophageal intubation is dangerous but manageable if recognized promptly.
- Many confirmation methods exist, but most lack reliability. Capnography is the gold standard.
- Video laryngoscopes greatly enhance safety, reduce the risk of esophageal intubation, and should be available in all clinical settings.
📚 References & Further reading
- American Society of Anesthesiologists. 2022 ASA Practice Guidelines for the Management of the Difficult Airway.
- Prekker ME, et al. Video versus Direct Laryngoscopy for Tracheal Intubation. New England Journal of Medicine. 2023.
- Lee DH, et al. Pitfalls of overreliance on capnography and disregard of direct visualization. 2024.
- “Confirmation of tube position” in Emergency Airway Management Clinical Guidelines (Royal Children’s Hospital, Australia)
- “Endotracheal Intubation with Video Laryngoscopy” — Practical Skills Manual / Airway guideline Milwaukee County
- Real-Time Trans-tracheal Ultrasound vs. Capnography for Intubation Confirmation in CPR Setting. PMC Article. 2024
- Point-of-care ultrasound for airway management in the emergency and critical care setting
- Lin J, et al. Point-of-Care Ultrasound in Airway Evaluation and Management. PMC. 2023.
- Chou EH, et al. Ultrasonography for confirmation of endotracheal tube placement: a systematic review and meta-analysis. ScienceDirect. 2015.
- Wheeler F, Espinosa J, Lucerna A, Gardecki J. The Application of Point-of-Care Ultrasound in ED Intubations and Airway Access: A Systematic Review. Rowan University Research Day Poster. 2021.
コメントを投稿するにはログインしてください。